I believe in the importance of a multidisciplinary approach when treating complex pelvic dysfunction and I am proud to say that I work with some of the most renowned experts and consultants in the Pelvic Health field. I will never hesitate to reefer and work along experienced colleagues to reach the best possible outcome in someone’s pelvic health.
What I treat ♂
I treat Men with a wide range of conditions that include but are not limited to the following. If you are in doubt, please email me here and find out if I can help you!
- Premature ejaculation
- Erectile dysfunction
- Sexual pain
- Hard flaccid syndrome
- Non-bacterial Prostatitis
- Post prostatectomy symptoms
- Chronic pelvic pain syndrome
- Tail bone and coccyx pain
- Pudendal neuralgia
- Bladder pain
- Stress urinary incontinence
- Idiopathic bladder overactivity
- Urgency
- Frequency
- Hesitancy
- Post void dribble
- Faecal incontinence
- Difficult defecation
- Painful evacuation
- Constipation
- Neurological pelvic dysfunction
- Cauda Equina Injury/syndrome
- Spinal cord injury
- Multiple Sclerosis
- Tarlov cyst
- Transverse Myelitis
- Pelvic nerve neuralgia
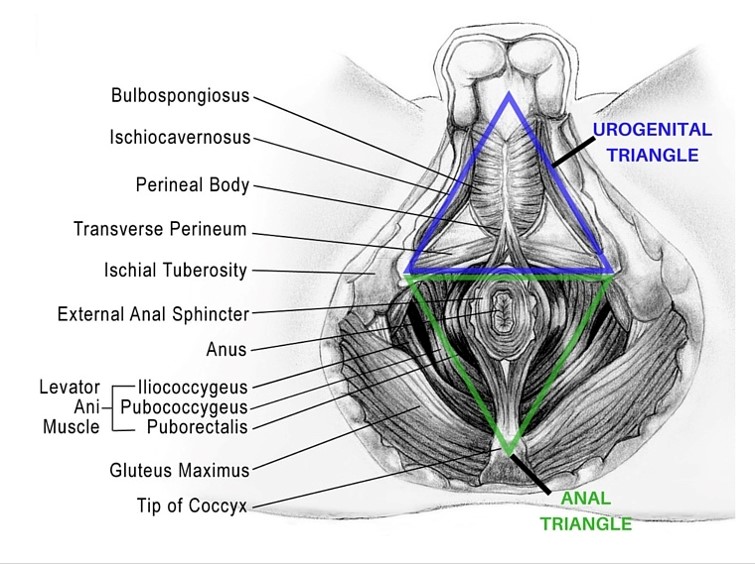
Male’s Pelvic Floor
Important facts and stats
- 1 in 9 men will experience incontinence in their lifetime
- 10-13% of the male population suffers with pelvic pain
- Chronic prostatitis/chronic pelvic pain syndrome— this accounts for about 90% of men with chronic prostatitis
- Studies have reported that approximately 1 to 5 percent of malepatients suffer from painful sex
- Premature ejaculation occurs in 25% of men between 25-65yrs
- Erectile dysfunction (ED) occurs in 14-28% of men under 40, in 1 in 5 of men over 40 and in 86% on men in their 80s
- There’s a high prevalence of ED in men with depression or lower urinary tract problems
- There is an association of ED prevalence with substance and alcohol abuse in young men.
- Urinary incontinence is not an isolated problem in men, but rather as a component of a multifactorial problem with other symptoms such as weak stream, hesitancy, and dribbling, or erectile dysfunction.
- Established risk factors predisposing men to urinary incontinence (UI) include increasing age, presence of lower urinary tract symptoms, urinary tract infections, functional and cognitive impairment, neurological disorders, and prostatectomy
- UI after radical prostatectomy is frequent, ranging from 2-57%. Rates steadily decline from the time of surgery and plateaus at 1 to 2 years
- Anal Incontinence is almost as common in men as in women
- The prevalence of overactive bladder is similar in men and women (female 16.0% vsmale 16.9%).
What I treat ♀️
I treat Women with a wide range of conditions that include but are not limited to the following. If you are in doubt, please email me here and find out if I can help you!
- Painful sex
- Vulvodynia
- Vestibulodynia
- Vaginismus
- Chronic pelvic pain
- Intersticial cystitis
- Endometriosis
- Chronic pelvic pain syndrome
- Tail bone and coccyx pain
- Pudendal neuralgia
- Bladder pain
- Stress urinary incontinence
- Idiopathic bladder overactivity
- Urgency
- Frequency
- Hesitancy
- Post void dribble
- Prolapse
- Faecal incontinence
- Difficult defecation
- Painful evacuation
- Constipation
- Prolapse
- Neurological pelvic dysfunction
- Cauda Equina Injury/syndrome
- Spinal cord injury
- Multiple Sclerosis
- Tarlov cyst
- Transverse Myelitis
- Pelvic nerve neuralgia
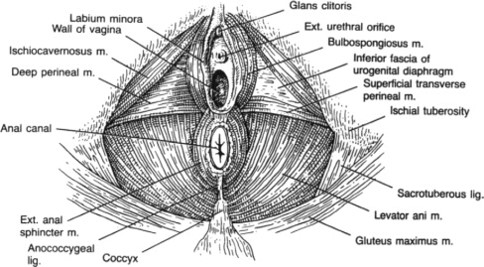
Female’s Pelvic Floor
Important facts and stats
- 1 in 3 women will experience incontinence in their lifetime
- Urinary incontinence occurring at least once in the past 12 months affects between 5 and 69% of women
- urinary incontinence affects 20-30% of young adult women, 30-40% of middle aged women, and 30-50% of elderly women
- The estimated prevalence of urinary incontinence in middle-aged and older women in the general population appears to be in the range of 30% to 60% (increasing with age)
- Pregnancy, labour and vaginal delivery (vs Caesarean section) are significant risk factors for later urinary incontinence
- Urinary incontinence is at least twice as prevalent in women as compared with men
- 1 in 4 women report painful sex in their lifetime
- 1:4 women will suffer from vulvodynia (vulval pain)
- 1 in 3 women will experience pelvic organ prolapse
- 400,000 people in the UK have interstitial cystitis, 90% of whom are female – 52% of women with interstitial cystitis / bladder pain syndrome report panic attacks and over 30% report depression
- The quality of life of bladder Pain patients is worse than patients experiencing chronic renal failure undergoing dialysis
- The prevalence of overactive bladder is similar in men and women (female 16.0% vsmale 16.9%).
- One in 10 women of reproductive age in the UK suffer from endometriosis
- The prevalence of endometriosisin women with infertility be as high as to 30–50%. Endometriosisis the second most common gynaecological condition in the UK
What to expect
Pelvic Health Assessment and Treatment
In a completely private setting, I will take your medical history and with as much detail as possible to determine the possible cause of your pelvic health problem. I may ask you to fill out a bladder, bowel and/or sexual health questionnaire to assess how your problem affects your quality of life.
During a physical examination, I will observe your posture, pelvic alignment, range of motion and mobility. With your consent, I will then test the sensation around your saddle area and I will test your pelvic floor muscle for tension, strength and range of motion by palpating your external and internal pelvic floor muscles. I will ask you to contract and release your pelvic floor. I will also ask you to cough and bear down to check your reflexes and coordination. This is by no means an absolute necessity but remains the gold standard for an accurate assessment of the pelvic floor muscles.
After a physical examination, I will design your individualized treatment plan. This may involve bladder training and bowel management, core and pelvic exercises, stretching, relaxation, deep breathing, visualization, biofeedback and electrical stimulation. I will use specialized manual therapy techniques to reduce muscle sensitivity and facilitate appropriate muscle activation. The length of the treatment and number of sessions required depends on multiple factors like how chronic your problem is, what your lifestyle is like and how committed you are to your physiotherapy plan.
Pelvic Health Treatment might include:
- Hands on manual therapy to your low back, abdomen and pelvis
- Trigger point therapy to reduce tension in the low back , hip and pelvic floor muscles
- Pelvic floor exercises to release your pelvic floor and/or to strengthening your pelvic floor
- Bladder training
- Specific hip, spine and pelvis exercises to get your pelvic floor moving better
- Specialized breathing and relaxation techniques
- Re-education of the pelvic floor, hip and abdominal musculature
- Pain management education
- Advice re sexual and toileting practices
- Home exercise plan and self-management
Book an appointment Now!
Get in touch
Please reach out to me if you have any questions or if you want to book your next appointment!